Introduction
Conversion disorder is a deviant somatic symptom where patients display deficits in voluntary motor or sensory function that is incompatible with neurological diseases (American Psychiatric Association, 2013). Prevalent rates of this disorder vary widely across cultures and the population studied (e.g., see Brown & Lewis-Fernandez, 2011; Feinstein, 2011). While the DSM-5 estimated the prevalence to be 2-5/100,000 (American Psychiatric Association, 2013), others reported somewhat higher rates (e.g., see Brown & Lewis-Fernandez, 2011). Prevalence is generally higher when clinical populations are sampled and it may vary between 1% to 14% (e.g., American Psychiatric Association, 2013; Brown & Lewis-Fernandez, 2011; Feinstein, 2011).
Despite tremendous theoretical and research efforts, the causes of this disorder and the process by which it develops remain a mystery (e.g., see Kanaan, Carson, et al., 2010; Rowe, 2010; Stone, Vuilleumier, & Friedman, 2010). Psychoanalytic theory, which initially coined the concept of conversion, attributes the cause of this disorder to repressed childhood trauma or unacceptable sexual or aggressive impulses (e.g., Breuer & Freud, 1895; Fenichel, 1946; Freud, 1894). However, studies refute the existence of repression (see review by McNally, Clancy, & Barrett, 2004; Piper, Lillevik, & Kritzer, 2008; Rofé, 2008), which constitutes the "cornerstone on which the whole structure of psychoanalysis rests" (Freud, 1914, p. 16). Many others question the soundness of "Freudian unconscious", the second pillar of the psychoanalytic theory of neuroses and claim that it needs to be abandoned (e.g., Greenwald, 1992; O'Brien & Jureidini, 2002; Rofé, 2008). Furthermore, although some investigators reported a relatively high rate of sexual abuse among conversion patients (e.g., Roelofs, Keijsers, Hoogduin, Näring, & Moene, 2002), others found this result among only a small minority of patients (6.6%; see Kuloglu, Atmaca, Tezcan, Gecici, & Bulut, 2003). Additionally, sexual abuse is associated with a wide range of other deviant behaviors (e.g., dissociative identity disorder, eating disorders, suicide and depression) yet about a third of those abused are found not to be affected (e.g., see review by Rofé, 2008).
Nevertheless, it might be premature to altogether abandon Freud's theoretical framework. A recent theory, the Rational-Choice Theory of Neurosis (RCTN; Rofé, 2010), shows that a new concept of repression and an alternative model of unawareness can explain in a more parsimonious way the development of neuroses and integrate all therapies relating to these disorders into one theoretical framework. Moreover, while Freud attributed neurotic symptoms to irrational forces, RCTN's theoretical achievement only became possible by incorporating Freud's idea, implicitly expressed in his theory, that neurotic disorders are, in fact, rational behaviors. As noted by Herbert Simon (1978), the late cognitive psychologist and Nobel Prize-winning economist,
it is perhaps … surprising to discover how pervasive assumptions of rationality are in psychoanalytic theory – confirming the suspicion that there is indeed method in madness. (p. 3)
Thus, the present article aims to demonstrate that RCTN, which regards neurotic disorders to be conscious and rational behaviors, can provide the most appropriate explanation for the development of conversion disorder. A secondary objective of this article is to suggest an improved model of self-deception by which, according to RCTN, unawareness of self-involvement occurs.
However, in order to provide an integrative theory of conversion disorder, RCTN needs to account for research supporting the behaviorist theoretical position (e.g., see Rimm & Somervill, 1977; Szasz, 1975; Ullmann & Krasner, 1975), the historical rival of psychoanalysis, that conversion disorder is intentionally adopted in response to current stressful demands (e.g., Ironside & Batchelor, 1945; Miller & Forbes, 1990; Mucha & Reinhardt, 1970; Rajmohan, Thomas, & Sreekumar, 2004).
It is also necessary to address studies suggesting that biological factors may be involved in the development of conversion disorder, which led some investigators to suggest changing its name to "functional neurological disorder" (e.g., Stone et al., 2011). These studies include: 1) Findings indicating abnormal cerebral functioning in conversion patients (e.g., Fink, Halligan, & Marshall, 2006; Rotge et al., 2009), such as an increased activity in the anterior cingulate cortex and associated regions in patients suffering from hysterical paralysis or paresis in their attempts, imaginary or real, to move the affected limb (e.g., de Lange, Roelofs, & Toni, 2007; Marshall, Halligan, Fink, Wade, & Frackowiak, 1997); 2) Research showing that hypnotic suggestions can produce behaviors similar to conversion symptoms, such as paralysis, and evidence indicating that hypnotic patients in these states display a similar pattern of neurological activity (e.g., Deeley et al., 2013; Halligan & Oakley, 2013); 3) Studies revealing that injury or physical illness frequently proceeded the onset of this disorder (e.g., Spierings, Poels, Sijben, Gabreëls, & Renier, 1990; Stone et al., 2009). A theory that attributes conversion disorder solely to psychological factors must provide an adequate explanation for the above indications that this disorder is at least partly controlled by biological causes.
One additional cardinal problem that needs to be addressed concerns the variability of conversion symptoms. If this disorder is indeed a homogenous type of deviant behavior that is controlled by the same mechanisms, it is necessary to explain how the wide variety of symptoms, such as paralysis, blindness, psychogenic movements, and seizures, are caused.
An additional challenge of an integrative theory of conversion disorder is to provide an understanding of how therapeutic change comes about. How is it that varied therapeutic methods, such as psychodynamic therapy (e.g., Viederman, 1995), behavior therapy (e.g., Blanchard & Hersen, 1976; Campo & Negrini, 2000; Goldblatt & Munitz, 1976) and drug therapy (e.g., Cybulska, 1997; Pu, Mohamed, Imam, & el-Roey, 1986; Voon, 2006; Voon & Lang, 2005), exert similar outcomes? Another puzzling issue, unexplained by traditional theories, concerns the efficacy of religious therapy (e.g., shaman) in the non-western countries and certain sections in the western society (e.g., Chowdhury, Nath, & Chakraborty, 1993; Witztum, Grisaru, & Budowski, 1996).
The Rational-Choice Theory of Neurosis: An Application to Conversion Disorder. Basic Assumptions
A New Conceptualization of Repression
RCTN agrees with Freud (1914) that repression is the key to understanding neurotic disorders, such as conversion disorder. However, given the numerous studies which refute the Freudian repression, RCTN suggests to maintain only the essence of this concept defined by Freud (1915) as "turning something away and keeping it at a distance, from the conscious" (p. 147). Thus, repression is seen as a conscious coping mechanism which deliberately eliminates threatening stimuli from attention through the employment of distractive maneuvers. This definition is consistent with Freud's original thinking since as noted by Erdelyi and Goldberg (1979), "The unconscious nature of repression was simply not a critical theme in Freud's treatment of the topic… in his very earliest writings (e.g., Freud, 1894) repression was treated as a potentially conscious mechanism… at least at times, repression is a conscious, deliberate act" (p. 365; see also Erdelyi, 2006). Moreover, the conception of repression as a conscious and deliberate withdrawal of attention is also consistent with the bulk of experimental studies which examined the nature of repression in a laboratory setting (see review by Holmes, 1974, 1990). Hence, this new definition restricts repression to a deliberate distraction, removing the other three components that comprise the psychoanalytic conception of this term, namely the forgetting of trauma, the unconscious, and the casual relationship between the forgotten trauma and neurotic disorders, as they have not received empirical support (see review by Rofé, 2008).
Another significant change made by RCTN is its distinction between normal repression and pathological repression. Normal repression refers to socially accepted means of distraction, such as reading or social activities. Repression becomes pathological when individuals are faced with stress that exceeds their coping abilities, to the extent that normal repression is insufficient for warding off stress-related thoughts. Under these circumstances, some individuals will consciously and rationally choose a neurotic behavior which heavily occupies their attention to the extent that they become unaware of their stressor. Thus, contrary to psychoanalysis, neurosis arises in response to current stressors, rather than historical events, and most importantly, repression is the consequence, rather than the cause, of neurosis.
Indeed, both research (e.g., Bhatia & Sapra, 2005; Malhi & Singhi, 2003; Mucha & Reinhardt, 1970; Sar, Akyüz, Dogan, & Öztü, 2009; Srinath, Bharat, Girimaji, & Seshadri, 1993) and case studies (e.g., Ironside & Batchelor, 1945; Lovinger, 2006) demonstrate that stress precedes the development of conversion disorder. These findings are consistent with the DSM's diagnostic requirement (criterion B) stating that "the initiation or exacerbation of the symptom or deficit is preceded by conflicts or stressors" (American Psychiatric Association, 2000, p. 492). However, as noted by Malhi and Singhi (2003) "the relationship between stressors and conversion symptoms is not immediately apparent during history taking and usually only a detailed psychosocial history and psychological testing is required…" (pp. 233-234).
Hence, conversion symptoms enable patients to ward off stress-related thoughts from their attention and thereby reduce the level of their distress. Accordingly, the name "conversion" needs to be preserved, despite the inadequacy of the psychoanalytic theory, since the preoccupation with the stressor is replaced with symptom-related thoughts. In Freudian terms, the individual's psychological energy is converted into preoccupation with a fictitious physical ailment.
Choice of Conversion Symptom
Similar to the consumer decision-making process (e.g., Wänke & Friese, 2005), RCTN claims that the choice of a specific conversion symptom is determined by three main principles: Needs, availability, and the cost-benefit analysis.
The Need of Controllability
Cumulative findings indicate that both humans and animals have a strong need to gain control over their life circumstances, and that lack of control has a detrimental cognitive, emotional, and physiological impact (e.g., Hofmann, 2005; Wellman, Cullen, & Pelleymounter, 1998; White, Lehman, Hemphill, Mandel, & Lehman, 2006). While some form of controllability is obtained through the distractive value of the symptom, research and clinical evidence indicate that people often choose a specific neurotic symptom if that behavior will enhance their ability to reduce the potential damage of the stress and/or motivate others to comply with their unique needs (see Rofé, 2000, 2010).
Accordingly, both research (e.g., Bhatia & Sapra, 2005; Grattan-Smith, Fairley, & Procopis, 1988; Ironside & Batchelor, 1945; Malhi & Singhi, 2003; Mucha & Reinhardt, 1970; Srinath, Bharat, Girimaji, & Seshadri, 1993) and clinical evidence (e.g., Blanchard & Hersen, 1976; Lovinger, 2006; Rajmohan, Thomas, & Sreekumar, 2004) indicates that patients usually choose a specific conversion symptom if it will enhance the individual's ability to escape a stressful situation. As noted by Dohrenwend and Dohrenwend (1969) regarding conversion symptoms developed by soldiers during World War II, "The patient's symptoms became his means to escape from further combat, and, not surprisingly, few recovered to the point where they could be returned to the front" (pp. 114-115). Similarly, Ironside and Batchelor (1945), who examined 40 aircrew members with ocular manifestations of hysteria during World War II, noted that "it is understandable that in pilots and other members of aircrews manifestations of hysteria should affect the eyes rather than the limbs, for what his legs are to an infantryman, his eyes are to a pilot" (p. 88).
Conversion symptoms may also be used to solicit attention and social privileges. For example, by developing hysterical blindness, a 15-year-old girl compelled her parents, who appeared very busy pursuing their own activities, to spend time with her reading her homework assignments (Grosz & Zimmerman, 1970). Similarly, in a case study of hysterical blindness (Brady & Lind, 1961), the patient succeeded, through a display of conversion symptoms, to put an end to the constant demands and criticisms of his wife and mother-in-law, which required him to work nights and weekends and perform various chores under their supervision. In the same way, Blanchard and Hersen (1976) described four case studies where conversion symptoms manipulated the social environment to provide the desired social rewards following stress that resulted from interpersonal conflicts (e.g., marital stress). Symptoms were abandoned when patients were "taught new ways of seeking and obtaining attention from the social environment" (p. 127).
Availability
Findings show that patients utilize their personal experiences to develop a conversion disorder that suits their coping demands. This may explain the fact that physical illness and injury are often reported among patients who subsequently developed conversion disorder (e.g., Jones, 1980; Merskey & Buhrich, 1975; Stone et al., 2009). Moreover, the symptoms are "commonly placed in some organ that was the site of a previous injury or disability" (White & Watt, 1981, p. 216; see also Mucha & Reinhardt, 1970; Weinstein, Eck, & Lyerly, 1969). Accordingly, Ironside and Batchelor (1945) reported that a significant number of military air crew members who developed ocular hysteria had a prior history of eye trouble. Similarly, as noted by Merskey and Buhrich (1975), "Patients who have epileptic fits may learn the pattern of their attacks and, when it is convenient to solve a conflict with this technique, they may use their knowledge of organic fits in order to develop hysterical ones" (p. 65). This is consistent with findings that show that 10% to 60% of patients with hysterical, non-epileptic seizures also suffer from true epilepsy (e.g., see Duncan, Oto, Martin, & Pelosi, 2006; Mellers, 2005).
Further evidence shows that 70% of conversion disorder patients had parents who suffered from illnesses in the same organs that were affected by their hysterical symptoms (Mucha & Reinhardt, 1970; see also Siegel & Barthel, 1986), and patients with non-epileptic seizures often have a family history of seizures (e.g., see Mellers, 2005). The choice of conversion symptoms may also become available through peer groups. For example, in their investigation of contagious hysteria among West Bengali women, Nandi, Banerjee, Bera, Nandi, and Nandi (1985) reported that episodes of hysterical seizures were usually precipitated by a husband beating his wife. As soon as the victim fell into a fit, other women suffering from similar stressors began to have hysterical seizures as well (for additional examples, see Chowdhury et al., 1993; Stevens, 1969; Ullmann & Krasner, 1975).
Cost-Benefit Analysis
In accordance with economic principles, human behavior is based upon rational calculations of cost-benefit in the interest of maximizing personal utility (e.g., Aumann, 2006; Becker, 1976; Lekachman, 1976; March, 1978; Simon, 1956). The incorporation of these ideas into psychology "may enable us to shed light on decisions which previously would have had to be classified as non-rational, irrational, or unexplained" (Williams & Findlay, 1981, p. 15). In fact, as noted before, Freud himself viewed neurosis as a goal-directed behavior rather than an arbitrary one. However, in Freud's theory the chosen symptom is to some extent unwise behavior (e.g., Dollard & Miller, 1950) as it is determined primarily by a past event. In contrast, RCTN attests that the symptom is developed in response to current stressful demands to help increase the individual's coping ability.
The principle of cost-benefit can also account for the low prevalence of conversion symptoms among men. Men tend to avoid these symptoms, as they would increase the risk of unemployment, which is far more threatening to them than to women (e.g., Artazcoz, Benach, Borrell, & Cortes, 2004). As noted by Sanborn (1990), men "overvalue their business powers to the exception of everything else, and this puts them at risk if their business falls apart" (p. 152). An additional factor is the lower social tolerance for weaknesses in men. Men are expected to be "independent, masterful, assertive, and instrumentally competent" (Eagly & Wood, 1991, p. 309), and to "repress emotions that might be associated with vulnerability" (Good, Sherrod, & Dillon, 2000, p. 64). Socialization processes encourage men "not to be sissies" (Sanborn, 1990, p. 151) and not "to express their desires for emotional support during stressful situations because it would be perceived as an inappropriate feminine coping strategy" (Eisler & Blalock, 1991, p. 50). The idea that gender differences in conversion disorder may be the result of cost-benefit considerations was also suggested by Jones (1980). Jones noted that considering the viewpoint of learning theory (i.e., reinforcement for appropriate behavior), psychoanalysis (i.e., primary and secondary gains), and sociological theory (i.e., culturally appropriate role models), "it is likely that the usefulness of conversion symptoms is greater for women, generally, than for men" (p. 436).
The cost-benefit principle also integrates research conducted by behavioral investigators showing that patients tend to abandon their symptoms either by reduction of the benefit (e.g., withdrawal of attention, monetary rewards, and hospital privileges) or by increasing the cost through punishment (e.g., see Blanchard & Hersen, 1976; Goldblatt & Munitz, 1976; Gooch, Wolcott, & Speed, 1997).
The Phenomena of Unawareness
The RCTN model of neurosis distinguishes between the patient's choice of symptom and the actual implementation of this behavior. The choice of a specific conversion symptom may be unconscious or spontaneous with no prior planning. However, the actual implementation of this choice is fully under conscious control. Nothing other than the conscious can impose complicated behaviors, such as hysterical paralysis and epileptic seizures, in the absence of neurological damages. The psychological processes by which patients spontaneously choose a specific conversion symptom and then become unaware of their conscious implementation of this choice are described below.
A) Intuitive Choice of the Symptom
Numerous studies indicate that decisions, problem-solving and judgments can be made in an analytic or an intuitive manner (e.g., see Dane, Baer, Pratt, & Oldham, 2011; Glöckner & Witteman, 2010; Hogarth, 2010; Kahneman, 2003; Pretz, 2008; Sarmány-Schuller, 2010). Unlike in an analytic choice, where the individual consciously examines the various options and relevant information before reaching a decision, an intuitive decision is made with little or no conscious awareness and thus is rapid and effortless. As noted by Hogarth (2001) an intuitive decision is "often experienced in the form of feelings (not words)…. The correlated are speed, and confidence … are reached with little apparent effort, and typically without conscious awareness … we know, but we do not know why [italics added]" (pp. 9-31). Similarly, Kahneman (2003) asserted that "a defining property of intuitive thoughts is that they come to mind spontaneously, like percepts" (p. 699; see also Sadler-Smith, 2008; Sinclair, Ashkanasy, & Chattopadhyay, 2010). Intuitive decisions are often taken in stressful situations "when an in-depth analysis is not possible and the decision-maker must move quickly to a plausible solution" (Sayegh, Anthony, & Perrewe, 2004, p. 183). Intuitive decisions are based on the individual's experiential resources stored in the long-term memory and usually are no less rational than conscious deliberate decisions (e.g., Glöckner & Witteman, 2010; Sayegh et al., 2004). Sayegh et al. noted in this respect that "theories of rationality have come a long way since Descartes proclaiming the superiority of cognitions. We now acknowledge that the human mind and the nature of our existence are defined by more than our ability to reason … rationality … [it] is partly defined through our ability to experience emotions … especially under crisis conditions…" (p. 196).
Based on the aforementioned studies and given the intolerable emotional state of the pre-neurotic patients, it seems likely that the choice of the specific symptom, determined by RCTN's three choice principals, is intuitive, i.e., with little or no conscious awareness.
B) Conscious Implementation of the Intuitive Choice
The integration of studies on intuitive choice is critical in understanding the unawareness of neurotic patients. However, the intuitive decision to choose certain behavior is, in and of itself, insufficient to account for a patients' unawareness of their Knowledge of Self-Involvement (KSI) in the conscious implementation of these choices. This state of unawareness is the consequence of two psychological processes: Creation of unawareness, caused by factors that facilitate the forgetting of KSI, and preservation of unawareness, that is obtained mainly through self-deceptive beliefs that prevent the retrieval of this information.
I) Creation of Unawareness: Forgetting of KSI. In order that patients will be unaware of the KSI, it must be recorded weakly in the individual's memory, thus its retrieval will be difficult. This necessary condition for the creation of unawareness is obtained immediately after the conscious implementation of the intuitive choice of the symptom through a number of factors that disrupt the encoding of KSI, along with several memory-inhibiting mechanisms that prevents its retrieval.
a) Encoding-Disrupting Factors.
-
Brief Exposure to KSI. One critical variable that determines the probability to forget the KSI immediately after the adoption of the conversion symptom is the duration of the patient's exposure to this information. This is consistent with evidence that the duration of exposure to a stimulus is a critical factor in determining the strength of the memory and thus the likelihood to forget this information (e.g., see DiNardo & Rainey, 1991; Memon, Hope, & Bull, 2003; Mensink & Raaijmakers, 1988). Indeed, clinical evidence indicates that patients' conscious exposure to the KSI is very brief as the conversion symptom is automatically implemented once this behavior is spontaneously chosen. One example of this process is a case of an unhappily married man whose wife became pregnant despite their agreement to remain without children (Malamud, 1944). On the way to the hospital to visit his wife and newly born child, the man was slightly injured in a car accident and spontaneously developed hysterical blindness. A second example (see Brady & Lind, 1961) concerns a 40-year old man who had trouble keeping even a semi-skilled job and was constantly harassed by his wife and mother-in-law on this matter. The patient received a small pension from the army for an eye infection which resulted in a partial loss of vision in one eye. While shopping for food with both women, he suddenly, without any precipitating event, became totally blind in both eyes. These occurred at a time when his wife and mother-in-law were unusually demanding, requiring him to work nights and weekends, and complete various chores under their supervision. Similarly, Masserman (1946) describes a 40-year old woman who suffered through several years of severe depression during an unhappy marriage. The woman tolerated being in this state until her favorite child died from an illness, when she suddenly developed a dissociative fugue. In another case (Abse, 1959), a man spontaneously developed total paralysis of his legs after his wife left him for another man. The husband had a strong impulse to pursue his wife in order to kill her and her lover, but the sudden paralysis prevented him from carrying out this impulse. In all of the above cases the symptom was chosen spontaneously without prior planning.
Why do patients automatically implement their intuitive decisions without carefully considering the negative consequences of the neurotic symptoms in terms of the serious disruption to their daily activities and the social embarrassment that they may cause? Here too, studies from the economic field conducted by Shiv and Fedorikhin (1999, 2002) can help to understand the seemingly irrational decisions of neurotic patients, such as those with conversion disorder. These researchers reported that when subjects are minimally preoccupied, choices are driven by higher cognitive processes and, as a result, they favor products that enable better long-term consequences (e.g., fruit salad). However, when subjects are maximally preoccupied, the decision-making process is controlled by "lower order affective reactions, arising from relatively automatic processes" (Shiv & Fedorikhin, 2002, p. 344). Consequently, individuals tend to spontaneously choose a product associated with an intense positive affective reaction, enabling short-term gratification (e.g., chocolate cake). Thus, since neurotic patients are intensively preoccupied with their stressors and suffer from a high level of emotional distress, they seek for an immediate discharge, overlooking the long-term harmful consequences.
-
Impaired cognitive functioning. Conversion patients often suffer from depression (e.g., Ballmaier & Schmidt, 2005; Shiri, Tsenter, Livai, Schwartz, & Vatine, 2003), and impaired attention (e.g., Brown, Poliakoff, & Kirkman, 2007; James, Gordon, Kraiuhin, & Meares, 1989; Roelofs et al., 2003). Other studies show that emotional distress distracts attention and interferes with the encoding process, resulting in poor learning and memory (e.g., Christopher & MacDonald, 2005; Roberson-Nay et al., 2006; Rose & Ebmeier, 2006). Considering these findings, it seems likely that the encoding of KSI is disrupted when the patient consciously decides to implement the intuitive choice of the symptom.
-
Intentional forgetting. KSI is anxiety-provoking information, since it reminds patients that they deliberately chose the symptom. Additionally, as stated previously, the symptom would have little distractive/repressive value if patients were to remain aware of their conscious involvement in this process. This means that patients are highly motivated in forgetting their KSI. Accordingly, since individuals possess the ability to disrupt the encoding of unwanted information (e.g., Anderson, 2005; Gottlob, Golding, & Hauselt, 2006), it can be assumed that once the conversion symptom is adopted they will deliberately direct their attention away from the KSI.
-
Symptom distractibility. The conscious implementation of the conversion symptom must intensively preoccupy the individual's attention, especially at the initial stage in which they experience a dramatic change in their behavior. This is consistent with Van Pelt's (1975) theoretical position, which noted that neurotic symptoms cause "super concentration of the mind, [inducing] a state of what may be called accidental hypnosis…. A patient suffering from a psychoneurosis behaves in every way as though under the influence of a post-hypnotic suggestion…" (pp. 28-29; see also Bliss, 1983, 1984). Furthermore, according to social cognitive theories of hypnosis which view this state as an intentional goal-directed behavior, individuals become unaware of the intentional production of the hypnotic behaviors by becoming fully absorbed in their goal-directed fantasies (see review by Lynn, Kirsch, & Hallquist, 2008). Therefore, considering RCTN's claim that conversion patients consciously implement their intuitive choice as a coping mechanism, it can be argued as in hypnosis, that here too patients become unaware of their KSI by intentionally focusing on the actual production of the conversion symptom. This is consistent with evidence indicating that patients with hysterical paralysis fail to display their symptoms when they are distracted (e.g., Cassady et al., 2005; Kihlstrom, 1994; Merskey, 1995; Spence, 1999).
Along the same lines, research data indicates that self-hypnosis (i.e., intense concentration) is in fact a central characteristic of various psychological groups (Bliss, 1980, 1983, 1984; Frankel, 1974). For example, a multiple personality patient, in describing her psychological state, observed that, "she creates personalities by blocking everything from her head, mentally relaxes, concentrates very hard … clears her mind, blocks everything out and then wishes for the person, but she isn’t aware of what she is doing" (Bliss, 1980, pp. 1392).
Accordingly, based on studies showing that encoding is often disrupted when attention is preoccupied by factors unrelated to the memory task (e.g., Tremblay, Nicholls, Parmentier, & Jones, 2005; Wolach & Pratt, 2001), here too the preoccupation with symptom-related stimuli should disrupt the encoding of KSI.
b) Retrieval-Inhibiting Mechanisms. Encoding-disrupting factors may not be sufficient to block the encoding of KSI into long-term memory. However, even if the KSI is weakly encoded, several memory-inhibiting mechanisms will significantly decrease patients' ability to retrieve this knowledge.
-
State-dependent memory. Given the controllability and distractive qualities of the conversion symptoms, it is expected that they will relieve the individual's emotional distress. Additionally, patients become preoccupied with symptom-related thoughts rather than with stress-related cognitions. Hence, based on studies indicating that retrieval becomes difficult when the individual's cognitive or emotional condition is different from that of the original learning situation (e.g., Eich, 1995; Eich, Macaulay, & Ryan, 1994), it can be assumed that patients' emotional and cognitive changes will inhibit the retrieval of KSI.
-
Suppression. Experimental findings by various groups of researchers show that people can intentionally inhibit retrieval of unwanted memories even after the encoding stage by reduced allocation of processing resources to this information (e.g., Anderson et al., 2004; Anderson & Green, 2001; Shane & Peterson, 2004). These findings are consistent with the psychoanalytic concept of suppression which was seen as the conscious effort to forget undesirable material (e.g., Freud, 1936). Accordingly, it seems likely that conversion patients can intentionally suppress the retrieval of KSI by directing their attention elsewhere.
-
Distraction. Distraction affects the individual's cognitive processes not only during the encoding stage but also at the retrieval of the encoded information. This claim is demonstrated in experimental studies on repression which initially claimed that material was forgotten due to unconscious repression but was in fact later discovered to be the consequence of distraction (e.g., see Holmes's review, 1974). Thus, the preoccupation with the dramatic change in behavior must be so intense that it should temporarily block, together with the aforementioned factors, patients' accessibility to their KSI.
II) Preservation of Unawareness: Self-Deceptive Belief. An additional factor that needs to be taken into consideration in the temporary creation of the unawareness, and most importantly in the preservation of this cognitive state, is patients' self-deceptive belief regarding the underlying causes of their symptoms.
Nisbett and Wilson (1977) noted that people have beliefs concerning the causal factors of various situations, which they acquire from their culture and employ to account for these events. Moreover, "people may be able to generate hypotheses linking even novel stimuli and novel responses" (p. 248). One cultural type of beliefs concerns the etiology of deviant behaviors, such as psychoanalytic thought in western society (e.g., Spanos, Weekes, Menary, & Bertrand, 1986) or spirit possession in less developed countries (e.g., Claus, 1979; Grisaru & Witztum, 1995; Kua, Sim, & Chee, 1986; Mischel & Mischel, 1958), which the individual incorporates through socialization (e.g., Ravenscroft, 1965) or other channels of information (e.g., reading or television; see Leonard, 1927, pp. 324, 410; McAndrew, 1989, p. 316; Spanos, Weekes, & Bertrand, 1985, p. 363). For example, as a result of Freudian's influence on western society, "many people learn to conceptualize interpersonal problems as resulting from an ‘unconscious process’ and as stemming from early negative experiences with parents" (Spanos, 1986, p. 300). Accordingly, it seems that conversion patients actively focus their attention during the actual implementation of the conversion symptoms on their culturally acquired belief and thus they further disrupt the encoding and retrieval processes of KSI. However, while this belief is one of several factors in the creation of unawareness (i.e., the forgetting of the KSI), it becomes exceptionally important in the preservation of this state immediately after the initial episode of the conversion symptom.
Given the rational nature of mankind, conversion patients may become preoccupied with questions posed by themselves or by others regarding the cause of their radical behavioral changes. This inquiry is anxiety-provoking for the patient since awareness of KSI would threaten the newly developed pathological coping mechanism. Patients succeed in preventing this threat by employing their self-deceptive beliefs. These beliefs become much stronger than at the initial adoption of the symptom as now patient are face with two types of validating evidence. One is the extrospective observation of a physical disability (e.g., hysterical paralysis), and the second is the introspective experience of loss of control (e.g., the inability to move a limb). This evidence will lead to a self-deceptive diagnosis of illness where patients believe that there is something physically wrong with them that are beyond their control. As a result, self-inquiry regarding the cause of the behavioral change will be focused on factors other than conscious involvement, and consequently the retrieval of KSI will be hindered.
Patients may also selectively focus on suitable information that can strengthen their self-deceptive explanation. As noted by Peterson and Djikic (2003), "we are always pursuing the limited goals we construe as valuable, from our particular idiosyncratic perspectives. We pay attention to, and remember, those events we construe as relevant, with regards to those goals. We do not and cannot strive for comprehensive, 'objective' coverage" (p. 88). Accordingly, "the hysteric misinterprets evidence and selectively attends to only a certain part of the overall evidence" (Bass, 2001, p. 139). For example, conversion disorder patients utilize the high prevalence of organic illnesses and physical injuries which were present prior to their disorder (e.g., Blanchard & Hersen, 1976; Jones, 1980; Merskey & Buhrich, 1975) to strengthen the belief that their symptoms are caused by biological factors (see also Stone & Sharpe, 2006). As noted by Weinstein et al. (1969), conversion disorder patients "stressed their injuries in the belief that they were etiologically significant" (p. 337; see also case studies by Brown et al., 2007; de Vignemont, 2009). An additional source of information that can strengthen patient's self-deceptive explanation is therapy. Patients tend to select a therapeutic intervention which is consistent with their belief, thereby increasing the strength of their deception (e.g., see Csordas, 1987). For example, Pattison and Wintrob (1981) noted in reference to spiritual possession that "concordance of belief systems of subject and healer concerning the causes and appropriate treatment of illness is usually the primary determinant of choice of healer" (p. 17).
The greater the individuals' knowledge of medicine the greater the difficulty of attributing the conversion symptoms to factors other than biological causes, therefore making it harder to obtain unawareness of KSI or self-deception. This may account for the fact that "conversion disorder has been reported to be more common in rural populations, individuals of lower socioeconomic status, and individuals less knowledgeable about medical and psychological concepts" (American Psychiatric Association, 2000, p. 495; see also Ahmad & Riaz, 2007; Deveci et al., 2007; Jones, 1980; Nandi, Banerjee, Nandi, & Nandi, 1992; Weinstein et al., 1969). For the same reasons uneducated people "are more likely to display dramatic or bizarre conversion symptoms [e.g., glove anesthesia; see White & Watt, 1981] based on primitive or religious notions" (Engel, 1970, p. 651; see also Viederman, 1995). More sophisticated people however will "manifest symptoms consonant with prevailing notions of physical illness" (Engel, 1970, p. 651; see also Jones, 1980).
Experimental findings showing that high self-deceptive individuals tend to ignore information indicating failure, despite the maladaptive consequence of their behavior (Peterson, DeYoung, et al., 2003), may seem inconsistent with the aforementioned clinical reports that conversion patients selectively attend to self-deceptive evidence indicating that they suffer from a physical illness. However, considering Peterson and Djikic's (2003) claim that people attend to events and experiences that construe as relevant to their motives and goals, it seems that while in the above experimental setting reduction of anxiety is obtained by ignoring failure experiences, conversion patients achieve this goal by attending to available experience that concur with their self-deceptive belief of illness.
III) Stabilization of Unawareness. The creation and preservation of unawareness discussed above concerns patients' unawareness of KSI at the initial presentation of the conversion symptom.
However since the conscious is the sole cognitive system responsible for the reactivation of the symptom it is necessary to clarify: a) Which situations cause patients to consciously reactivate their symptoms? b) How do patients succeed in remaining unaware of KSI, despite repeated displays of this behavior?
a) Symptom Reactivation Situations.
-
Stress. One situation which causes patients to reactivate their symptom is stress. This reaction enhances both their ability to repress/distract stress related thoughts and to exercise control over the stressor. For example, Blanchard and Hersen (1976) described a case of a 14-year-old girl who developed aphonic hysteria following a quarrel with her mother of which she spontaneously recovered in several weeks. However, when she subsequently quarreled with one of her sisters and was severely scolded by her mother, her voice was reduced to a whisper. A full relapse occurred when the mother sharply questioned the patient about her sexual relationships with her cousin. In another case, the reactivation of the subject's conversion symptom coincided with a variety of environmental stressors. "Among these were his role as 'housewife,' difficulties with his 18 year-old son, being discharged from the National Guard after 20 years of service, and his strong opposition to his youngest daughter's marital plans" (Blanchard & Hersen, 1976, p. 124). Similarly Benzick (2001) mentions a case of a 17-year-old female who suffered from pseudo-seizures, and whose symptom was worsened in the presence of the stressor (her father). Likewise, Nandi et al. (1985) reported that a patient with hysterical seizures usually displayed her symptom when she was beaten by her husband.
-
Belief-challenging conditions. The second situation that causes the reactivation of the symptoms is belief-challenging conditions. The self-deceptive belief is crucial for preserving unawareness of KSI and for providing a rationale for maintaining the symptom. Accordingly, it is expected that challenging the patient's self-deceptive belief will cause the reactivation of the symptom. Failure to do so may invalidate the belief, and therefore threaten the patient's ability to maintain the symptom. This theoretical position can account for an experimental study by Levy and Jankovic (1983). In this study, a hysterical patient displayed a variety of dramatic pseudo-neurological symptoms when given a placebo, which she believed it to be a certain drug that, according to her medical knowledge, should intensify her symptoms. Thus, the patient was obliged to consciously display her symptom because failing to do so would sabotage her self-deceptive belief and, consequently, the maintenance of her pathological coping mechanism.
In another experimental study (Grosz & Zimmerman, 1965; Zimmerman & Grosz, 1966), a patient suffering from hysterical blindness identified the presence or absence of visual stimuli below the chance level. The experimenter manipulated the patient's behavior through a collaborator by telling him that the doctor thought he could see and that a truly blind person identifies a higher number of correct responses than chance-level performance. As one would expect, in a subsequent visual test, the subject’s correct responses increased to chance level. Here too, when the self-deceptive belief was threatened, the patient adjusted his symptomatic behavior accordingly.
-
Demand Characteristics. Another condition that causes the return of the symptom is the demand characteristics of the faked "illness". Thus, patients suffering from psychogenic movement must routinely display their symptom at a certain frequency, and must activate it soon after waking from sleep. Failure to do so would challenge their self-deceptive belief of illness, and may be interpreted by others either as faking or as their condition not being serious. The same claim is true for hysterical paralysis and hysterical blindness where they must routinely behave in a similar way to people suffering from true paralysis or blindness. Hence, the hysterically paralyzed patient must consistently display his handicap whenever the effected limb is in use, such as washing or going to the bathroom.
b) The Deceptive Cycle. Figure 1 describes the self-deceptive cycle where patients consciously reactivate the symptom in response to the aforementioned three situations and repeatedly cause themselves to be unaware of KSI. Basically, the same psychological processes, which were involved in the creation and preservation of unawareness at the initial adoption of the symptom, are repeated in each new display of this behavior. At this stage, however, unawareness of KSI occurs at a much faster rate due to two factors which were absent in the initial adoption of this behavior. One is the automatic reactivation which gradually becomes like a conditioned reflex. This automatization is the consequence of both practice (i.e., repeated display of the symptom) and emotional relief (i.e., reinforcement) caused by the distractive and controllability values of this behavior. The automatic display of the conversion symptom reduces the amount of attention allocated to both the decision to reactivate this behavior as well as to its actual performance, and consequently the awareness of KSI. This explanation is consistent with Lynn et al. (2008) claim' who noted with regard to hypnosis that
Once an intention to respond a suggestion is formed, it is no longer requires much conscious control. Instead, the response is triggered as an automatic or quasi-automatic operation that intervenes in initiating, correcting, interrupting, inserting, continuing and terminating action (p. 126).
This effect is also shown in the unconscious performance of motor skills which is attributed to the reduced amount of attention allocated to the execution of these behaviors as a result of practice (e.g., Kihlstrom, 1987; Lewin, 1982; Moore & Stevenson, 1991; Morris, 1981).
Studies on motor skills which show that minimal attention is always necessary for an adequate performance (e.g., Reason, 1983, 1984a, 1984b) can also help us to understand the previously mentioned evidence (see p. 8) that conversion patients failed to display their symptoms when attention was diverted (e.g., Cassady et al., 2005; Kihlstrom, 1994, p. 382; Merskey, 1995; Spence, 1999). Additionally, although the reactivation of the symptom becomes automatic, patients can regulate the presentation of the symptom in order to reduce potential damage (e.g., see Leary, 2003; Mischel & Mischel, 1958; Nicol, 1969), and can even stop their behavior when the cost exceeds the benefit (see Blanchard & Hersen, 1976; Goldblatt & Munitz, 1976).
The second factor disrupting the encoding of KSI is self-deceptive belief. Once established, the belief becomes a powerful distractive tool which, like the symptom itself, hinders the encoding of KSI. The self-deceptive cycle by which patients become unaware of their conscious involvement at each new presentation of the same symptom is presented below.
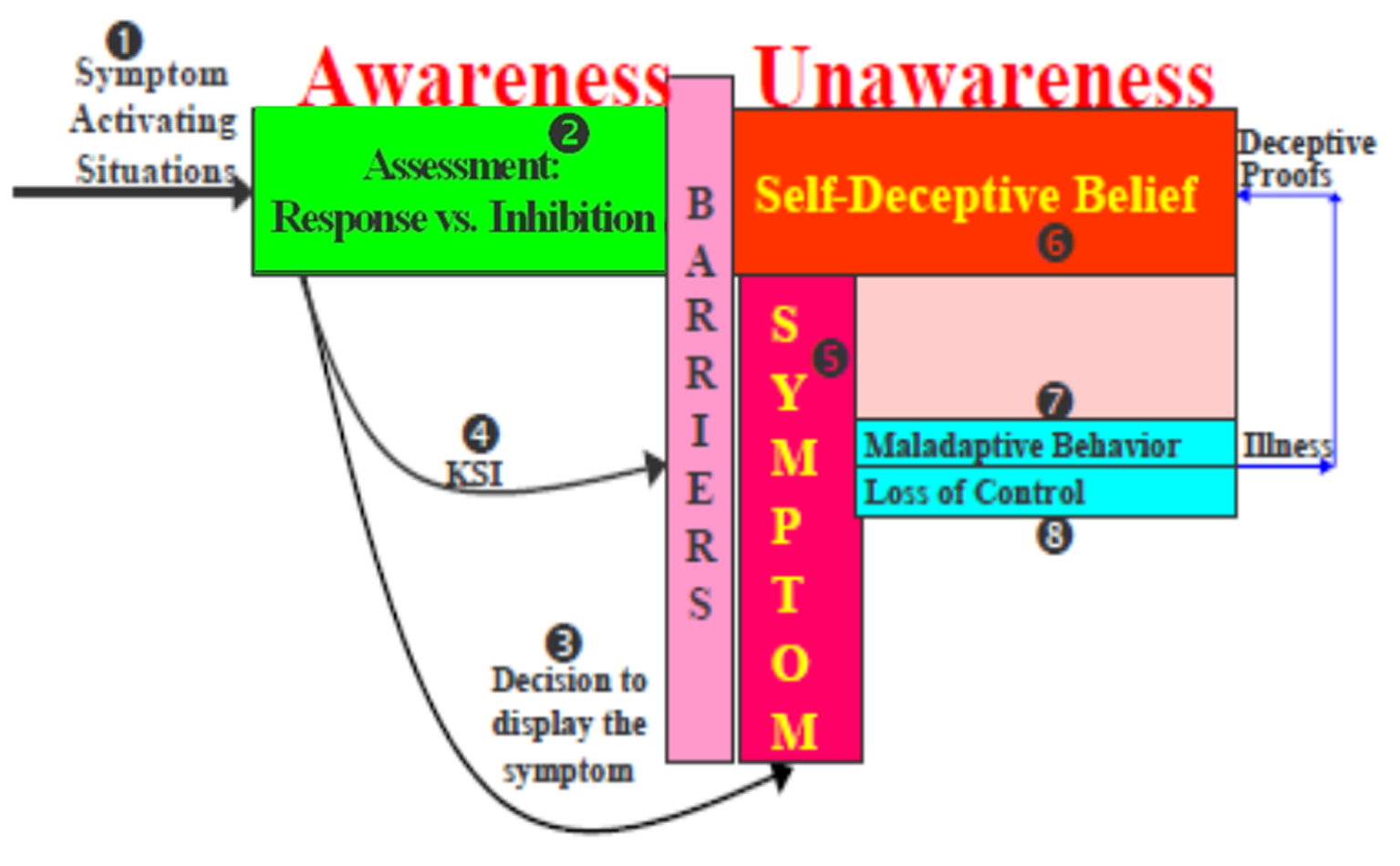
Figure 1
The dececptive cycle.
No. 1 in Figure 1 refers to three situations that stimulate the conscious re-activation of the symptom: stress, belief-challenging conditions, and symptom demand characteristics. No. 2 relates to the automatic reactivation of the symptom where the patient modifies or inhibits the display if rapid assessment indicates potential damage. Nos. 3 & 4 represent the automatic release of the symptom and patients' minimal awareness of KSI, respectively. Nos. 5 & 6 represent the self-deceptive belief and the symptom which constitute the two barriers that block the accessibility of KSI through their powerful, distractive effects. Hence, like hypnosis where individual becomes unaware of the intentional production of their hypnotic state by focusing on the hypnotic suggestion and their behavioral change (e.g., see Lynn et al., 2008), the intense preoccupation with the symptom and self-deceptive belief enables patients to direct their attention away from KSI. Two additional memory-inhibiting factors are intentional forgetting and state-dependent memory caused by substantial emotional and cognitive changes. Once unawareness is created as a result of the aforementioned factors, patients are faced with the same psychological state to which they were exposed immediately after the initial display of the symptom. One is the observation of maladaptive behavior in the form of physical symptoms and the second is the introspective experience of loss of control (Nos. 7 & 8, respectively). Hence, these two observations reconfirm that the patient is physically ill, which constitutes a new deceptive proof that revalidates patients' initial self-deceptive belief.
Explanation of the Functional Neurological Findings. The deceptive cycle can shed light on previously mentioned studies, where hysterically paralyzed patients displayed antagonistic neurological activities, of both activation and inhibition when they were instructed to move their affected limb. While biologically oriented investigators interpreted these reciprocal neurological activities as a genuine inability to move the affected limb, RCTN attributes these findings to the physiological concomitants of contradictory conscious messages. The first message is the conscious decision to move the affected limb when instructed to do so (Nos. 3 & 4), which stimulates the brain area responsible for the moving. The second message is the simultaneous employment of the self-deceptive belief of the illness to inform the brain of an inability to move the affected limb. This explanation may account for van Beilen et al. (2010)'s statement "I want to move my arm, but I cannot" (p. 156). Thus, the antagonistic brain activities in the aforementioned studies parallel to the antagonistic conscious messages. This theoretical position can also account for the previously mentioned studies showing that hypnotic suggestions of limb paralysis produce similar pattern of neurological activities when attempting to move the affected limb (e.g., Deeley et al., 2013; Halligan & Oakley, 2013). This neurological evidence does not necessarily support the mechanistic explanation of conversion disorder or hypnosis. As noted by Lynn et al. (2008), in reviewing studies relating to cognitive theories on hypnosis, "all subjective experiences are assumed to have physiological substrates or correlates with potentially identifiable brain activity" (p. 128).
Inadequacy of Rival Models of Unawareness. RCTN is not alone in accounting for conversion disorder by using the concept of self-deception; however, none of other models can adequately address patients' unawareness. For example, Sackeim and Gur (1978; see also Gur & Sackeim, 1979) developed a psychoanalytic model of self-deception stating that under certain motivational conditions, individuals can maintain two contradictory beliefs, one of which remains outside the conscious. In support of this theory they found that subjects, who had experienced failure, were unable to identify their own voices heard from a recording device, while simultaneously displaying elevated levels of GSR (Galvanic Skin Response). This theoretical model was then applied by Sackeim, Nordlie, and Gur (1979) to account for a case study of a hysterically blind girl, previously reported by Grosz and Zimmerman (1970), who supposedly held two contradictory cognitions: (1) the patient consciously believed herself to be blind; and (2) she "unconsciously knew" that she was not blind, because she accurately identified visual objects in 480 experimental trials. In other words, from the standpoint of Sackeim et al., hysterically blind patients can display accurate visual performance without actually being aware that they can see.
However, Sackheim et al.'s position is complicated by the fact that the girl never claimed to be totally blind. "Her behavior showed no signs of any visual deficits except when asked to read small or large print . . . [and] she scored 100% loss of vision for reading in both eyes" (Grosz & Zimmerman, 1970, pp. 118-121). This evidence suggests that the girl suffered from selective hysterical blindness similar to air force patients in World War II who complained of selective ocular hysteria (Ironside & Batchelor, 1945). The latter authors reported 40 cases of aircrew members who exhibited visual disturbances (e.g., blurred vision or defective night vision) that prevented them from fulfilling flight-related tasks. According to Ironside and Batchelor (1945) these patients suffered from problems related to "looking" rather than from disturbances in "seeing". In looking, "the interference is with the will of the patient, and such functions as perception, appreciation, attention and response are involved; in other words it is the patient who is at fault, and not his visual mechanism" (p. 89). Thus, it appears that the aforementioned girl deliberately failed to read by consciously disrupting the focus of her eyes. The patient could simultaneously eliminate KSI from her conscious and reinforce her self-deceptive belief of physical illness based on this seemingly objective evidence of blurred vision and the sense of introspective evidence of lack of control of the physical "defect", as specified in Figure 1. This coping strategy enabled the girl to compel her parents, who "appeared to be very busy pursuing their own activities and seemed always to be in a rush to go somewhere or work on some project" (Grosz & Zimmerman, 1970, p. 117), to fulfill their parental duties (e.g., helping with homework).
Kanaan (2010), addressing the difficulty in distinguishing between conversion disorder and malingering, noted that "it may make perfect sense to consider hysteria as a form of deception, without the ethical implications we associate with lying" (p. 55). According to Kanaan hysteria is a form of deception where the patient has no intention of influencing others' beliefs or behaviors, as opposed to lying "where I intend through my assertion to make you believe something that I think is false" (p. 57). However, Kanaan ignored studies showing that increasing the cost of the conversion symptom motivates patients to abandon their deviant behaviors, which indicates that these behaviors are intentionally adopted. Moreover, he did not clarify how patients become unaware of the underlying causes of their symptoms.
A more systematic theoretical approach to the issue of self-deception among the general population in everyday life was made by von Hippel and Trivers (2011). However, it is difficult to see how their self-deception model, which constitutes an important contribution to the understanding of everyday life, can promote the understanding of neurotic behaviors such as conversion disorder. One of the challenging problems of this model is that "one cannot deceive oneself into believing something while simultaneously knowing it to be false" (Bandura, 2011, p. 16). RCTN resolve this problematic issue by stating that patients initially forget (i.e., become unaware) of their KSI and then, immediately afterward, validate a self-deceptive belief on the basis of an extrospective observation that their behavior is maladaptive and an introspective experience of loss of control. It is also difficult to see how such explanation could integrate the various therapeutic interventions relating to conversion disorder, as this is demonstrated below.
As stated, according to cognitive theories of hypnosis, subjects experience the hypnotic behavioral changes as involuntary occurrences, though they are goal-directed behaviors, mainly because they become fully absorbed in the hypnotic suggestions (Lynn et al., 2008). Thus, one may argue that cognitive theory of hypnosis can account for the unawareness of conversion patients without postulating the brief exposure to KSI. However, hypnosis is not a continuous state of behavioral change that may last for an extended period of time where the individual repeatedly displays this change as in conversion disorder. Moreover, hypnotic theories would have difficulty to account for the efficacy of therapy.
Therapy
One of the most difficult issues that challenge traditional theories of psychopathology is their inability to integrate findings relating to the success or failure of different therapeutic interventions into a single theoretical framework (e.g., see reviews by Feixas & Botella, 2004; Lampropoulos, 2000, 2001). In the absence of such an integrative theory, investigators in the field focused on empirical evaluations of therapeutic techniques, neglecting to address the underlying mechanism of change. Consequently, while some believe that that all therapies have similar efficacies, and suggested that a number of common factors, such as therapeutic alliance, empathy, support and emotional catharsis are responsible for therapeutic changes (e.g., see Feixas & Botella, 2004; Lampropoulos, 2000; Luborsky et al., 2002; Reisner, 2005), others lists a number of empirically supported therapies (ESTs), claiming that they have been found to be more effective than other therapies for specific disorders (Chambless, 2002; Reisner, 2005).
However, one of most central goals of traditional theories of psychopathology was to uncover the underlying mechanisms of therapeutic change, and as noted by Tryon (2005) "the absence of empirical support about these theories… does not diminish the need for an explanatory context" (p. 68). As noted by Power and Brewin (1997),
some therapists simply bury their heads in the sand and continue with their favorite techniques. Others, like ourselves, are puzzled and are asking if there are common mechanisms that apply across different therapies that might explain both their effectiveness and their (sometimes) lack of effectiveness? (p. xi).
Similarly, Tyron (2005) stated that "[the] effectiveness of efforts to persuade clinicians to adopt ESTs may depend substantially on the extent to which science can explain why ESTs work and thereby provide clinicians with an empirically supported explanatory context in addition to effective interventions" (p. 68).
RCTN has already proven its integrative approach (Rofé, 2010) due to its ability in accounting for the differential efficacy of various therapeutic methods pertaining to neurosis, such as behavior therapy, religious therapy, cognitive-behavioral therapy (CBT), psychodynamic therapy and drugs, using one set of theoretical principals. Each of these therapies obtains its efficacy by affecting different mechanisms which according to RCTN maintain the specific symptom. The purpose of this section is to demonstrate the integrative utility of RCTN with specific regard to conversion disorder.
Behavior Therapy: Removal of the Controllability
As specified before, punishment procedures, such as withdrawal of attention or the application of noxious stimuli, motivate patients to abandon their conversion symptoms (e.g., Blanchard & Hersen, 1976; Campo & Negrini, 2000; Goldblatt & Munitz, 1976). While behaviorists account for the efficacy of this therapy by learning concepts, RCTN attributes it to the disruption of the cost-benefit equilibrium of the symptom. Once the symptom ceases to be beneficial, patients are motivated to consciously abandon their symptom. However, symptom substitution or relapse is likely if patients lack the ability to cope with the stressor following behavior therapy which coerces them to abandon their pathological coping mechanism (e.g., see Blanchard & Hersen, 1976; Chou, Weng, Huang, & Chen, 2006).
Religious Therapy: Sabotaging Self-Deceptive Belief
Another therapeutic intervention which is commonly used in non-western countries and certain sections of western society is religious therapy (e.g., see Alonso & Jeffrey, 1988; Endrawes, O'Brien, & Wilkes, 2007; Razali, 1999; Wijesinghe, Dissanayake, & Mendis, 1976; Witztum et al., 1996). It seems that the efficiency of this treatment results from the psychological power of a religious figure to sabotage the patients' ability to deceive themselves that the symptoms are maintained by supernatural forces beyond their conscious control. In other words, when individuals attribute their symptoms to supernatural forces, the most preferable therapeutic intervention would be a prestigious religious figure of the same faith who leads the patient, using certain religious rituals, to the conviction that he was freed from these evil forces. Resistance to believe in the efficacy or authority of the religious figure would be considered heresy. Consequently, once the deceptive function of the self-deceptive belief is sabotaged, it would be difficult for patients to rationalize the prolongation of the symptom and thus increase their tendency to abandon it.
For example, Razali (1999) described a case of a 38-year-old female Malaysian Muslim, who suddenly developed hysterical paralysis after her husband had taken a second wife. She was unsuccessfully treated by a number of traditional healers and medical practitioners, before agreeing to participate in a popular Malaysian "spirit-raising séance (Main Puteri), which lasted 3 days. The patient's symptom was completely removed on the third day of the "performance", which was attributed to the departure of the "evil spirits" from her body. Thus, since the patient deceived herself that her symptoms were controlled by evil forces and also believed that the "therapist's" rituals "cured" her from these forces, she could no longer rationalize the maintenance of her deviant behavior and therefore she was obliged to abandon it. Three additional case studies of conversion disorder in which religious rituals, including the recitation of passages from the Qur'an and offerings of a goat's head or a number of eggs, had a curative effect are described by Kok (1975).
Psychodynamic Therapy: Removal of Distraction
There is no empirical evidence to support the psychoanalytic claim that the efficacy of this treatment results from the lifting of repression, i.e., awareness of the childhood traumatic events (see review by Bachrach, 1996; Barber & Lane, 1995; Charman, 2003; Rofé, 2008). Moreover, some researchers attribute this outcome to the placebo effect (e.g., see Grünbaum 1986, 2002). As noted by Jopling (2001), psychodynamic-insight therapies, including Freudian and neo-Freudian psychoanalysis, do not provide authentic self-knowledge. Rather, they are "highly susceptible to generating placebo insights, that is, illusions, deceptions and adaptive self-misunderstandings that convincingly mimic veridical insight but have no genuine explanatory power". (p. 19).
Nevertheless, RCTN maintains the psychoanalytic fundamental idea of removal of repression (Rofé, 2010) only if therapy increases patients' insight to the current stressor rather than childhood trauma. Once a patient becomes aware of their current stressor, which is the underlying factor that motivates the adoption and maintenance of the symptom, this behavior loses its distractive value and increases the patient's wilingness to abandon it. For example, Temple (2001) treated a hospitalized 15 year old girl suffering from hysterical limb paralysis, using the psychodynamic interpretative method. The patient was in a conflict with her mother concerning her sexual autonomy. The conversion symptoms allowed her to distract her attention from the source of her conflict (i.e., the autonomy over her sexuality), distance herself from her mother (i.e., the stressor) and manipulate her parents to provide sympathy and attention through hospitalization. The psychodynamic interpretive therapy focused on the patient's current stressor and thus increased her awareness of the underlying causes of her behavior. Consequently, the symptom lost its distractive value and "enabled her to find more appropriate ways of recognizing her feelings and the necessity for her to be paralyzed gradually reduced" (p. 292). However, since the patient did not have sufficient coping abilities, she redisplayed her pathological coping mechanism, i.e., conversion symptom, "when she was under stress or when a discussion about her return home took place" (p. 292).
In another case study (Viederman, 1995), the son-in-law of a 68-year old orthodox Jew and successful businessman influenced the local Rabbi to exclude his father-in-law from the synagogue. Knowing the father-in-laws aggressive temperament and fearing that he might do "something destructive to his reputation", the family decided to send him on a trip to Florida. Upon his return when he learned about the family's "conspiracy", he developed conversion symptoms expressed by rigidity of the legs and weakness in the neck muscles. From RCTN's standpoint, the symptoms improved the patient's emotional condition as they enabled him to: a) repress his angry feelings resulting from his perception of his family's "subversive" behavior and their "los[s] of confidence in him"; b) rationalize his absence in the prayer services at the synagogue; and c) receive sympathy and support from his wife, children, and perhaps even from the community members.
The brief psychodynamic interpretative method, consisting of 6 weekly meetings, was aimed to increase the patient's awareness of his current stressor. For example, the patient was told "You have been unable to walk, because you are afraid to walk into the synagogue. You are afraid of how angry you are. Your confidence has been undermined... I think your symptom will go away with this knowledge. Now get up, and walk around the room comfortably and without the cane" (p. 406). The increased awareness of the stressor decreased the distractive/repressive value of the symptoms, and thus increased the patient's tendency to abandon these behaviors. Additional factors which contributed to the therapeutic outcome were the therapist's suggestions, encouragement and sympathy as well as the participation of his wife in therapy, where the couple "spoke openly and freely to one another of their affections and their dissatisfactions" (p. 405).
Stress Management
Given RCTN's claim that current stress is the underlying cause of conversion disorder, it would appear that the removal of stress would motivate patients to abandon their symptom. For example, Iglesias and Iglesias (2009) described a case of a 17 year-old boy held in a juvenile detention center, who developed hysterical leg paralysis once he was informed of his transfer to a reputedly violent unit. Shortly after announcing that this particular unit was full and consequently all transfers would be redirected to other units, he spontaneously recovered. In a another case, an 11 year-old girl developed a loss of peripheral vision in her right eye after witnessing her alcoholic father beating her mother and being ordered by the father to "keep her eyes glued to the television" and "not to stare at what went on." Shortly after the intervention of Child and Family services, which apparently addressed the patient's stressor, the child's symptoms were completely remitted. Similar clinical evidence indicating that the removal of stress results in spontaneous remission of conversion symptoms was illustrated in two case studies by Leary (2003).
Since stress plays a crucial role in the development of conversion disorder, it is essential to strengthen the patients coping skills. Otherwise, symptomatic therapy such as behavior therapy may result in symptom substitution. For example, Blanchard and Hersen (1976) described a number of case studies where symptom substitution occurred after a symptom was successfully removed through behavioral therapy. Effective and long lasting therapy was secured only when this therapy was accompanied by coping skills training. In their concluding remarks, the author noted that:
It would appear that because of a faulty learning history this type of patient has not developed the requisite social skills needed to cope with both the usual and more unusual stresses encountered in life. Therefore, training or retraining in social skills becomes a needed ingredient in a comprehensive therapeutic regime. (p. 127)
Drug Therapy
Since depression is relatively high among conversion disorder patients (e.g., Goldstein & Mellers, 2006; Menza, 1989; Sar et al., 2009; Voon & Hallet, 2006), and given RCTN's claim that the symptoms are defense a against intolerable levels of emotional distress, it is expected that the reduction of depression using antidepressants would motivate patients to abandon these behaviors. The very few studies which examine the effect of this treatment with conversion patients are consistent with this expectation (e.g., Cybulska, 1997; Pu et al., 1986; Voon, 2006; Voon & Lang, 2005). However, since drug therapy does not address the underlying causes of the symptom, i.e. current stressors, it is likely that discontinuation would result in a relapse. While this is true with other neurotic disorders (for a review see Rofé, 2010), there is no evidence to evaluate the validity of this claim with regard to conversion disorder.
Another type of drug therapy found to be useful in the treatment of conversion disorder is abreaction, which involves interviewing patients under the influence of a drug. A systematic review using the meta-analysis method shows that this type of treatment may be beneficial for acute and treatment-resistant conversion disorder (Poole, Wuerz, & Agrawal, 2010). In their attempt to account for this efficacy, Poole et al. (2010) noted that "the use of suggestions augmented by the drama of the procedure is likely to raise the expectancy of recovery and challenge dysfunctional health beliefs [italic added] that cause and maintain the condition" (p. 93). Thus, from RCTN's perspective, abreaction treatment may be effective as it helps to sabotage the patient's self-deceptive belief. However, this type of treatment may be harmful if the patient lacks adequate coping skills to address the increased level of depression which the abandonment of the symptom may cause. For example, Menza (1989) observed a 31 year-old male, who developed hysterical leg paralysis following severe depression caused by a laminectomy surgery which produced no improvement to his chronic back pain. The patient refused to accept that his symptom had resulted from psychological problems and was therefore given a drug abreaction interview to facilitate recall of repressed materials. Although the patient's symptom temporarily disappeared, one hour later he was found attempting suicide. After three days of physical restraint and sedatives for behavioral control, the leg paralysis returned and he remained paralyzed during the two month follow up.
From RCTN's standpoint, the drug abreaction interview sabotaged the patient's self-deceptive belief that his symptoms were the consequence of organic cause. Indeed the patient "insisted that his ability to walk was merely the effect of the drug on his legs” (p. 137), which indicates that the drug was effective because it sabotaged his belief that the symptom was the consequence of organic damage. Thus, the patient abandoned his symptom because he could no longer rationalize the maintenance of his symptom. Once he lost his pathological distractive coping mechanism, the depression returned motivating his suicide attempt and the re-manifestation of the symptom.
Placebo
Sometimes individuals may wish to rid themselves of their symptoms either because the stressor no longer exists or because they have adjusted to it. However, they may hesitate taking such action because they must explain to themselves and others the dramatic "cure". Under such conditions, the mere participation in a therapy can provide the patient a self-deceptive excuse to rationalize the abandonment of a symptom. As noted by Ullmann and Krasner (1975):
Once the person has made the act, and performed the new role, he cannot shift back into his prior role…This is one reason why a placebo may be effective: It gives the person an "out," saves face and avoids many of the aversive consequences in "giving up" the "sick" behavior. (p. 256; see also Mooney & Gurrister, 2004).
For example, when Carl Gustav Jung (1963) informed a middle-aged female patient, who had been suffering from hysterical paralysis for many years, that he was going to hypnotize her, the patient immediately fell into a deep trance, before the therapist started the process. She talked without pause for over a half-hour, resisting Jung's attempts to awaken her. Soon afterward she declared herself cured, threw away her crutches and proceeded to walk. Jung, whose theoretical framework could not account for this unexpected result, announced to his students, "Now you've seen what can be done with hypnosis" (p. 120). However, he noted that "in fact I had not the slightest idea what had happened" (p. 120). From RCTN's standpoint, it seems likely that after so many years of suffering from the fake symptoms, the stressor was either removed or she adjusted to it. The symptom became a burden and Jung provided her with the deceptive excuse required to abandon this behavior.
Discussion
As shown, RCTN's intuitive-intentional model of neuroses succeeded to integrate seemingly incompatible observations by rival theories into a single theoretical framework. This includes: 1) Freud's clinical observations that neurotic patients repress the underlying causes of their disorders and that they are unaware of the mechanism that controls their behavior; 2) Behaviorists' claims that conversion disorder is merely role-playing that aims at either escaping stressful situations or motivating others to comply with their unique needs; 3) Neurologists' studies indicating abnormal cerebral functioning, such as when hysterically paralyzed patients display antagonistic neurological activities when instructed to move their affected limb; and 4) Findings showing that illnesses and injuries often precede the development of conversion disorder.
RCTN also accounts for several other issues that are unexplained by traditional theories, such as gender and educational differences in the prevalence of conversion disorder, and factors affecting the heterogeneity of conversion symptoms. Additionally, RCTN has resolved the confusion regarding the name of "conversion disorder". The adoption of this disorder enables patients to eliminate/repress stress-related thoughts from their attention as it replaces their stress-related thoughts with illness-related symptoms. Hence, despite radical differences between RCTN and psychoanalysis with regard to the concept of repression, in both theories "conversion" is the most appropriate term. Furthermore, like psychoanalysis, RCTN claims that a necessary condition for the understanding of neuroses, such as conversion disorder, is to account for patients' lack of awareness to the underlying cause of the radical change in their behavior. However, RCTN attributes this effect to the intuitive choice of symptoms, the rapid conscious implementation of this spontaneous suggestion, and several factors that disrupt the encoding and memory of KSI along with the self-deceptive belief that preserves this state of unawareness.
This new insight into the mechanisms through which patients' unawareness concerning the causes of their symptoms constitutes an important factor in understanding the process of therapeutic change, and in accounting for the successes and failures of various therapeutic methods pertaining to neurosis. Although this issue was already discussed in the original paper (Rofé, 2010), the present article focuses specifically on conversion disorder and thereby demonstrates the integrative ability of RCTN using much greater amount of relevant research and clinical evidence.
One may argue that the idea that conversion symptoms are intentional eliminates the distinction between malingering and this disorder, and contradicts the DSM's diagnostic requirement that the conversion symptom "is not intentionally produced or feigned" (American Psychiatric Association, 2000, p. 492). However, as noted by Delis and Wetter (2007), "many clinicians are reluctant to use diagnoses such as Malingering, Factitious Disorder, and Conversion Disorder at least in part because of difficulty in objectively assessing the presence or absence of intentionality in the generation of the excessive symptom" (p. 593). Similarly, Krahn, Bostwick, and Stonnington (2008), noted that "the task of determining whether the actions the patient takes is feigning illness or intentional, voluntary, conscious or unconscious, is problematic in that these behaviors represent an ‘untestable diagnostic hypothesis for many cases'" (p. 278). These arguments, which are becoming more common, strengthen Miller's (1999) earlier claim that the distinction between malingering and conversion disorder is worthless, and have led current investigators to suggest that the DSM requirement for "the exclusion of feigning [as a diagnostic criteria for conversion disorder] should be dropped" (Kanaan et al., 2010, p. 428). Indeed, in its latest version, the DSM abandoned the aforementioned requirement as now it states that "the diagnosis of conversion disorder does not require the judgment that the symptoms are not intentionally produced (i.e., not feigned)…" (American Psychiatric Association, 2013, p. 320).
Nevertheless, despite these justified critiques, it would be mistaken to neglect clinicians' impression, since Freud, that conversion patients are unaware of the mechanism that controls their behavior. Therefore, instead of the DSM's unempirical diagnostic criterion, a more precise description of patients' cognitive state would simply be unawareness, i.e., patients' inability to account for the underlying causes of their radical change in behavior. An additional criterion that may help to distinguish conversion disorder from malingering is whether the behavioral change is response to an extreme level of stress, as is typical to conversion disorder, or that the response is motivated by a desire to obtain some valuable social rewards
A further issue that worth discussion concerns the DSM-5's (American Psychiatric Association, 2013) decision to add the name functional neurological symptom disorder to conversion disorder. Although this name was proposed by some researchers that reviewed the relevant data (e.g., Stone et al., 2011), there seem to be little scientific justification for this suggestion. The overall evidence, particularly studies showing that the same pattern of seemingly abnormal cerebral activities were also observed in hypnotic subjects and that psychological interventions cause the removal of the conversion symptoms, dismiss the possibility that biological factors have any involvement in causing this disorder.
A more problematic issue is the DSM-5's decision to reclassify conversion disorder as somatic symptom disorder in light of the growing dissatisfaction to DSM-III's decision to categorize it as somatoform disorder (e.g., Dimsdale & Creed, 2009; Jablensky, 1999; Kanaan et al., 2010; Mayou, Kirmayer, Simon, Kroenke, & Sharpe, 2005; Noyes, Stuart, & Watson, 2008; Stone et al., 2011). In re-evaluating the scientific validity of this decision it is worthwhile to consider the harsh critiques against the DSM. Researchers argued that the DSM's classifications were implicitly affected by medical models so that it was never truly as atheoretical as it claimed to be, that these categories were determined by consensus rather than by data, that the task force consisted of mostly psychiatrists rather than representatives from the main schools of thought, and that the decision to remove neurosis was affected by political and economic pressures from pharmaceutical and insurance companies (e.g. Burstow, 2005; Follette & Houts, 1996; Pilecki, Clegg, & McKay, 2011; Warelow & Holmes, 2011). Moreover, even if the DSM would have been atheoretical, such diagnostic approach is undesirable and it may hinder the scientific progress (e.g., Acton & Zodda, 2005; Grinker, 2010; Follette & Houts, 1996). As noted by Grinker (2010) "without the structure of underlying explanations, the manual became a list of symptoms for an expanding list of diseases, from a few dozen disorders in the first edition to well over 200" (p. 169). Similarly, Warelow and Holmes (2011) noted that now the DSM contains "three times as many disorders as it did in 1952, and it is more than seven times longer than the first edition" (p. 385).
Further, the DSM-III decided to exclude neuroses as a diagnostic category because the task force arrived at the conclusion that "there is no group of conditions which together comprise the 'neuroses'" (American Psychiatric Association, 1976, p. 11). However, based on research and clinical evidence RCTN has demonstrated in its original version that neuroses not only share five empirical criteria that can effectively separate neuroses from other disorders (Rofé, 2000, pp. 98-118) but also accounts for the development and treatment of these disorders using a single set of theoretical concepts (Rofé, 2000, 2010). Therefore, taking the aforementioned arguments into account, we should consider the reinstatement of neuroses as a diagnostic category and conversion disorder its sub-category. From this standpoint, it seems that the DSM-5's decision to classify conversion disorder as Somatic Symptoms and Related Disorders along with the new diagnostic category "Psychological Factors Affecting Other Medical Conditions" is most unfortunate. While the former is a coping strategy that patients intentionally adopt when facing intolerable levels of stress, the essential feature of the later is "the presence of one or more clinically significant psychological or behavioral factors that adversely affect a medical condition by increasing the risk for suffering, death, or disability" (American Psychiatric Association, 2013, p. 322).
The DSM's biased attitude towards medical models and its antagonism towards psychoanalytic theory is also reflected by its attempt to rationalize the categorization of conversion disorder, which according to the DSM itself is "medically unexplained" (p. 310), together with medical conditions, such as diabetes, cancer and coronary disease, that have a clear medical cause but were exacerbated by psychological factors. The DSM's rational for this decision is as follow:
The reliability of determining that a somatic symptom is medically unexplained is limited, and grounding a diagnosis on the absence of an explanation is problematic and reinforces mind-body dualism. It is not appropriate to give an individual a mental disorder diagnosis solely because a medical cause cannot be demonstrated (p. 309).
Thus, although evidence supporting the medical models is lacking and many findings reviewed in this article seriously question the likelihood of this possibility, the DSM favored the position of these models. Furthermore, while it is true that research seriously questions the validity of psychoanalysis (e.g., Rofé, 2000, 2008), which maintains the mind-body dualism (e.g., see Carella, 1974), it seems that Freud's approach made a more valuable contribution to the understanding of conversion disorder and neuroses in general than rival theories. Although RCTN radically differ from psychoanalysis in many fundamental respects, it was essentially Freud's line of thought that enabled RCTN to gain a comprehensive understanding of conversion disorder.
It can be argued that RCTN does not meet the scientific criteria for the acceptance of a new theory, as it lacks supportive evidence of its own. However, although the original article provides a case study demonstrating the efficacy of RCTN's therapeutic method (Rofé, 2010), the acceptance of a new theory does not necessitate new supportive data. Researchers in the philosophy of science noted in this respect that the ability of a theory to explain existing data is even more important than its ability to present new supportive evidence (e.g., Brush, 1989, 1990, 1992, 1993, 2005; Proctor & Capaldi, 2001; see also Haig & Durrant, 2002). As claimed by Brush (1989) "a successful explanation of a fact that other theories have already failed to explain satisfactorily … is more convincing than the prediction of a new fact, at least until the competing theories have had their chance (and failed) to explain it" (p. 1127). Similarly, Tryon (2005) noted that although hypothesis testing is undoubtedly important "at some point the resulting facts need to be placed into explanatory context. Mature sciences provide explanatory theories in addition to making testable predictions" (p. 69). In support of this claim, Proctor and Capaldi (2001) noted, in reference to the new idea of Plate tectonics, which placed existing geological data into a coherent explanatory context, that European colleagues accepted Plate theory well before the American geologists as they valued explanation as well as prediction whereas American scientists limited themselves to prediction and testing hypothesis. Additional example demonstrating the importance that science places on explanation is the fact that "Darwin's evolutionary theory remained on the margins of biology approximately 75 years until population genetics provided the missing causal explanatory mechanisms" (Tryon, 2005, p. 69).
Moreover, according to Snyder (1994; see also Schlesinger, 1987) the difference between prediction and explanation is a mere technicality. Although the necessary condition for the acceptance of a new hypothesis is evidence, it makes no difference whether this became available before (explanation) or after (prediction) the formulation of the theory. From this standpoint many research findings could in fact be predicted by RCTN. One example is the aforementioned evidence that hysterical paralyzed patients fail to display the symptoms when their attention is diverted (e.g., Cassady et al., 2005; Kihlstrom, 1994, p. 382; Merskey, 1995; Spence, 1999) or when awakened during sleep (e.g., Lauerma, 1993). Another example is the research and clinical evidence, such as the experimental study by Levy and Jankovic (1983) specified above, showing that challenging patients' self-deceptive belief motivates them to redisplay their conversion symptoms. Both types of studies could be predicted by RCTN and it is difficult to see how these findings can be explained by rival theories.
At this stage it is difficult to specify rigorous ways in which RCTN could be tested. One way that may also expand the theoretical domain of RCTN is to examine the efficacy of RCTN's rational insight therapy (Rofé, 2010) compared to psychoanalytic intervention. Like Freud, RCTN claims that the best therapeutic intervention is insight, whereby therapy increases patients' awareness to KSI. While in some exceptional cases effective results can be obtained by telling patients at the very early stage of therapy that they intentionally adopted their symptoms (see Merskey, 1979, pp. 264-265), usually such type of intervention is likely to cause strong resistance. Insight's intervention may be more fruitful after establishing therapeutic trust by exposing patients, individually or in a group, to various theoretical options and lead them to a conclusion using the Socratic questioning method, that RCTN provides the best explanation for their symptoms. A control group can be conversion patients that are led through the same methodology into believing that psychoanalytic theory is most appropriate explanation and that childhood trauma, such as repressed sexual abuse, is the underlying cause of their symptoms. After creating their respective insights, both groups will be given coping skills training to face their respective stressors. Two dependent variables can be used to examine the validity of RCTN: 1) Examining brain activity of hysterical paralyzed patients when attempting to move their affected limb. These measures can be taken at the beginning of the experiment and immediately after creating the respective insight before addressing their stressors using coping skills training. It is expected that a significant reduction in inhibitory brain activity will be seen in RCTN's group rather than in the psychoanalytic subjects; 2) Reduction in conversion symptoms which will be more significant in the RCTN than the psychoanalytic group.
In conclusion, despite the profound differences, RCTN can be seen being similar to psychoanalysis as both view neuroses as a unique diagnostic category and the clarification of the mechanisms by which patients become unaware of the underlying causes of their symptoms as the key to the understanding these disorders. Also, they both conceive these disorders as goal-oriented behaviors. Furthermore, RCTN preserves the essence of Freudian repression and replaces the unconscious with the model of self-deception. At this stage, this approach seems the best integrative model for the explanation of conversion disorder.
 This is an open access article distributed under the terms of the Creative Commons
Attribution License (
This is an open access article distributed under the terms of the Creative Commons
Attribution License (